Elevated inflammation is a risk factor for many psychiatric (e.g., depression) and somatic conditions (e.g., rheumatoid arthritis). Inflammation is influenced by psychosocial processes such as emotion regulation. Characterization of which emotion regulation characteristics impact inflammation could help refine psychosocial interventions aimed at normalizing health-harming inflammatory activity for individuals with psychiatric and somatic illnesses. We systematically reviewed the literature on associations between a variety of emotion regulation traits and inflammation.
Out of 2816 articles identified, 38 were included in the final review. 28 (74%) found that (a) poor emotion regulation is associated with higher inflammation and/or (b) strong emotion regulation skills are associated with lower inflammation. Consistency of results differed as a function of the emotion regulation construct investigated and methodological characteristics. Results were most consistent for studies testing positive coping/social support seeking or broadly defined emotion regulation/dysregulation. Methodologically, studies testing reactivity to a stressor, adopting a vulnerability-stress framework, or using longitudinal data were most consistent. Implications for integrated, transdiagnostic psychoimmunological theories are discussed, as well as recommendations for clinical research.
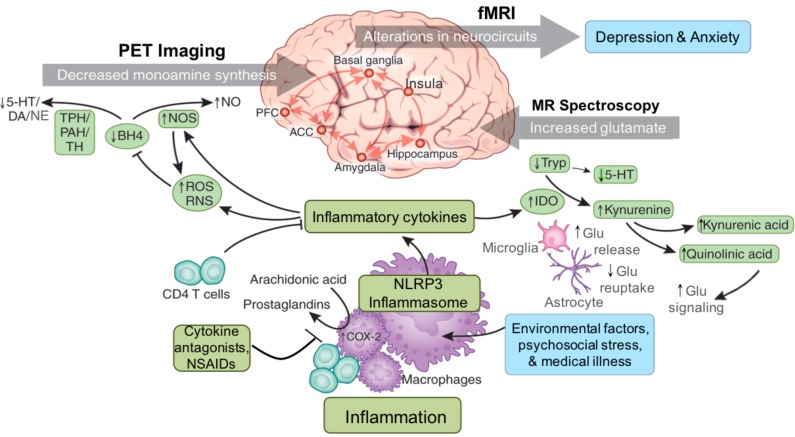
Inflammation is a transdiagnostic correlate of many medical and psychiatric conditions (Dantzer et al., 2008, Michopoulos et al., 2016, Pearson et al., 2003, Saccaro et al., 2021, Sattar et al., 2003). Further, evidence suggests that inflammation has a causal effect on some of these health outcomes including depression (Capuron and Miller, 2004, Knight et al., 2022, Kuhlman et al., 2018, Moriarity et al., 2020), ulcerative colitis (Ek et al., 2021), and osteoarthritis (Ek et al., 2021), positioning it to be a potentially important treatment target for a variety of disorders. Although inflammation-modulating biological treatments such as non-steroidal anti-inflammatory drugs, interferon-α therapy, and minocycline generally are considered primary interventions for inflammation-mediated conditions, psychosocial interventions such as cognitive-behavior therapy (CBT) and mindfulness meditation also have been shown to influence inflammatory biology (Black and Slavich, 2016, Shields et al., 2020). Inflammatory malleability to these biological and psychological interventions affords patients who suffer from inflammation-mediated disorders flexibility in treatment options. For example, biological interventions might be a useful adjunctive when individuals with both depression and elevated inflammation are struggling with the cognitive demands required to engage in evidence-based psychotherapy. Conversely, individuals for whom anti-inflammatory medications are contraindicated—or who refuse medication for other reasons—may benefit from psychosocial interventions (Shields et al., 2020).
Yet, the mere understanding that psychosocial interventions (e.g., cognitive-behavioral therapies) influence inflammation is insufficient to maximize therapeutic impact. It is necessary to explore which treatment targets of extant psychosocial interventions actually affect inflammatory biology. A nuanced understanding of which specific characteristics of psychosocial treatments reduce inflammation would have direct implications for treating inflammation-mediated mental and physical health problems and could help advance precision medicine approaches aimed at reducing risk for these conditions. Further, this work would integrate inflammatory mechanisms into existing, psychosocially oriented theories of psychiatric risk and resilience, which would guide theory development (Moriarity, 2021) and advance understanding of many complex, multifactorial health conditions.
Increasing the quantity and quality of emotion regulation skills, and decreasing emotional reactivity, is a shared goal of many psychotherapies (e.g., CBT, dialectical behavioral therapy, acceptance and commitment therapy), as strengthening emotion regulation aptitude can reduce distress in various areas of psychosocial functioning (Beatty et al., 2016, Ma and Fang, 2019). Indeed, skillful emotion regulation is associated with improved communication and social relationship functioning overall (Vater and Schröder, Abé, 2015). Additionally, individuals with advanced emotion regulation also are better able to select strategies that best align with their goals within the situational context (English et al., 2017). Given that inflammatory biology is reactive to increases in negative affect such as anger or anxiety (Carroll et al., 2011), it is plausible that improved emotion regulation also could influence inflammatory biology.
In fact, there are several extant theories/models implicating emotion regulation as a modulator of inflammation. The perseverative cognitions hypothesis is not specific to inflammation, but describes how perseverative (e.g., rumination, worry) reactions to unpleasant situations or emotions can simultaneously amplify the magnitude and duration of the physiological stress response-exacerbating downstream consequences for basal stress biology (Brosschot et al., 2006). Our team has extended this work to include cognitive vulnerabilities more generally in an immunocognitive model of psychopathology (Moriarity et al., 2018)-attempting to clarify discrepant results in stress/arousal→inflammation research by including emotion-modulating cognitive vulnerabilities as a moderator of this association. Others have described emotion regulation traits/abilities as a mediator of the negative emotionality→inflammation pathway (Renna, 2021) and suggested the possibility of bidirectional feedback loops between negative emotions, inflammation, and health outcomes. Although comprehensive tests of bidirectional relationships are lacking in this area, there is evidence from studies involving experimentally-administered endotoxin that inflammatory activity might increase negative reactivity (Dooley et al., 2018) and that certain health sequelae of inflammation (e.g., depression) are also predictive of future increases in inflammation (Moriarity, Kautz et al., 2020).
A few reviews have explored the relationship between emotion regulation and inflammation for specific emotion regulation constructs (e.g., see Szabo et al., 2022 for a scoping review on rumination and inflammation), but there have been no attempts to systematically review how a wide variety of emotion regulation characteristics are related to inflammatory biology. Given the range of both emotion regulation characteristics and inflammatory proteins, a systematic review of the associations between these two constructs is an important contribution to the field insofar as it would point to the therapeutic processes that are most relevant for reducing inflammation, a key health-damaging process. This is especially important given that the identification of cognitive targets that impact inflammatory biology could lead to the development of more precise psychological interventions for a variety of inflammation-mediated health outcomes (Moriarity, 2021).
We addressed this need by systematically reviewing for the first time all of the available evidence for associations between various emotion regulation characteristics and circulating inflammatory proteins in clinical (i.e., medical and psychiatric) and nonclinical samples. In addition to identifying which emotion regulation characteristics are associated with inflammatory biology, we assessed contextual factors that might influence the presence or absence of theoretically consistent associations to the extent possible (e.g., emotion regulation tested as a moderator of arousal-related characteristics and inflammation, emotion regulation as a trait vs. in the context of acute stress). Then, the reviewed evidence is used to formulate recommendations for clinical practice, and the integration of inflammation into theories of emotion regulation and psychopathology.
Article originally appeared in Neuroscience & Biobehavioral Reviews Volume 150, July 2023, 105162

